Even though orthopedic implants have a good biocompatibility, adverse local tissue reactions (ALTRs) can occur. Historically, ALTRs were first associated with failed metal-on-metal (MoM)1,2 bearings and were recorded as early as 1988.3 However, ALTRs have also been described with other implant modifications such as metal-on-polyethylene (MoP)4, ceramic-on-polyethylene (CoP)5, ceramic-on-ceramic (CoC)6 and ceramic-on-metal (CoM)7, disproving the hypothesis that ALTRs are only caused by MoM bearings, emphasizing the complexity of this clinical topic.
The terms pseudotumor, aseptic lymphocyte-dominated vasculitis-associated lesions (ALVAL), trunnionosis and metallosis have been interchangeably used in the literature to describe ALTRs in the clinical setting.8 A pseudotumor describes the presence of benign aseptic masses and bursae, whereas ALVAL is a histologic description for a specific tissue appearance. Trunnionosis refers to tribocorrosion damage at the femoral head-neck junction, whereas metallosis describes the stained appearance of the joint capsule and periprosthetic tissues due to large amounts of metal debris.8,9 The term adverse reaction to metal debris (ARMD) is a subset of ALTR but only refers to adverse reactions to metallic debris.8 However, all the above listed terms are primarily descriptive terms from evidence-based observations in the clinical setting but cannot be validated as clinical coding systems for specific diagnoses of ALTR-related revision surgeries.
Based on major national arthroplasty registries, ALTR in periprosthetic soft- and bone tissue can be defined as an inflammatory tissue reaction, which is often accompanied by aseptic loosening and osteolysis of the periprosthetic bone. The development of ALTRs can be multifactorial but is mostly associated with the implant material itself and with the presence of corrosion- and implant wear particles in periprosthetic tissue. Cellular responses to wear and corrosion particles in periprosthetic tissue are driven by either the innate or adaptive immune system, leading to chronic tissue inflammation. Implant wear particles activate macrophages, which form multinucleated foreign body giant cells and trigger an inflammatory tissue response, leading to the migration of further immune cells, especially lymphocytes in the state of chronic inflammation. In addition, T lymphocytes have been described to trigger a delayed type IV hypersensitivity reaction to metal debris. Other factors such as surgical procedures and patient-related factors may further favor and/or exacerbate the development of ALTR.10-12
The development of ALTRs in periprosthetic tissues is multifactorial, and the underlying causes and mechanisms are often complex and difficult to understand. The presence of implant debris and metal corrosion products is usually, but not exclusively the cause for the development of chronic inflammation and ALTRs. The choice of implant material is crucial but does not guarantee the prevention of ALTRs. Furthermore, the usage of implant modifications with different materials further complicates the prediction of ALTR development. Moreover, because there is no consensus on the definition and terminology of ALTRs, their clinical diagnosis and the decision for revision surgery are difficult to make. Additionally, tissue inflammation and intoxication as well as severe osteolysis pose a major clinical challenge for the revision surgeon.
This article presents three case reports of ALTRs with different implant materials and modifications that demonstrate the complexity of ALTRs and the clinical challenges for the revision surgery.
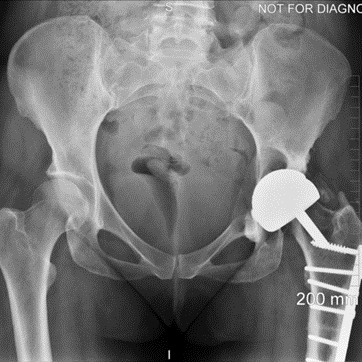
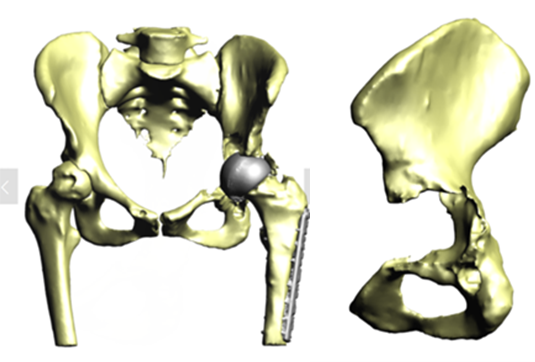
The patient, a 49-year-old woman, underwent metal-on-metal (MoM) hip resurfacing procedure in 2001 due to a unilateral hip dysplasia (DDH). 17 years later, she presented with mild hip pain but extensive loss of bone in the pelvis which was presumably caused by an inflammatory reaction to metal wear debris. Her blood metal ion levels were 100 times higher (cobalt 188 bbp and chromium 126 bbp) than from patients with well-functioning MoM hips.
The case posed multiple challenges. The patient was at imminent risk of pelvic fracture without surgery. However, surgery itself also risked fracture of the pelvis during implant removal. Furthermore, the remaining pelvic bone was poisoned by metal debris and thus the patient’s bone integrity was compromised, which could affect the stability of a new implant.
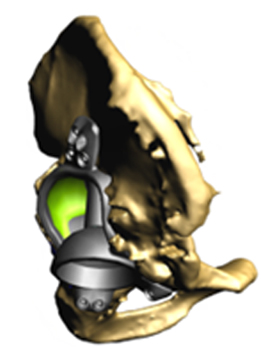
A multidisciplinary team decided that revision surgery was necessary due to the risk of fracture and very high metal ion levels. The plan involved removing the existing MoM implant and fitting a custom 3D-printed acetabular cup. The procedure required meticulous care to avoid causing fractures during implant removal. The new cup would only be effective if the pelvis remained intact.
The operation was successful, with minimal bone loss during implant removal. A custom-made titanium acetabular cup was fitted and stabilized with screws. Postoperative imaging confirmed correct implant positioning and satisfactory fixation. The patient’s recovery was positive, with significant reductions in metal ion levels and the restoration of pain-free hip function.
This case represents ALTR with MoM, which was characterized by extensive osteolysis of pelvic bone, which was presumably caused by metal wear debris. Elevated blood levels of chromium and cobalt further supported this hypothesis.
This case demonstrates the importance of precise surgical planning and execution in complex hip revision surgeries. The use of 3D-printed implants tailored to the patient's anatomy greatly improved the chances of successful fixation despite significant bone loss. Update at 6 years post operative is that the patient living a full and active life with excellent hip function. More details about this type of surgery has been published by Professor Hart:
Di Laura, Anna PhD; Henckel, Johann MD; Hart, Alister FRCS(Orth)a. Custom 3D-Printed Implants for Acetabular Reconstruction: Intermediate-Term Functional and Radiographic Results. JBJS Open Access 8(2):e22.00120, April-June 2023. | DOI: 10.2106/JBJS. OA.22.00120
Source: Revision of a metal on metal hip with massive acetabular osteolysis and previous femoral osteotomy using a custom 3D-printed cup in a mid-life woman — Complex Hip Surgery - CASE 10
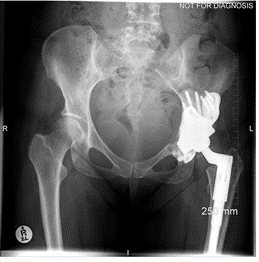
This case involves a 67-year-old gentleman who faced a series of complications due to hip trauma he had experienced over 50 years ago. After his primary and revision surgeries, and subsequent three hip replacements, he was left with a failing hip implant. His most recent hip replacement lasted 13 years before massive circumferential acetabular osteolysis caused the cup to loosen. Imaging revealed anterior and medial wall deficiencies, while the posterior column remained intact. The patient had a metal-on-polyethylene (MoP) bearing, which over time led to the wear of the polyethylene liner, triggering an inflammatory reaction and bone loss due to polyethylene debris.
The surgical plan required a custom 3D-printed acetabular cup, designed specifically for the patient's anatomy. The implant was designed with three flanges for optimal fixation. The surgery involved a posterior approach, with meticulous bone preparation to minimize further bone loss and ensure the custom implant fit securely.
This case represents ALTR with MoP. ALTR was characterized by massive osteolysis of the pelvic bone, which was most likely caused by polyethylene wear debris. This case underscores the complexity of revision hip surgeries and highlights the value of custom 3D-printed implants for achieving secure fixation and improving patient outcomes despite significant bone loss. Update at 7 years post operative is that the patient has excellent hip function and more can be seen in this paper:
Durand‐Hill, M., Henckel, J., Di Laura, A., & Hart, A. J. (2020). Can custom 3D printed implants successfully reconstruct massive acetabular defects? A 3D‐CT assessment. Journal of Orthopaedic Research®, 38(12), 2640-2648.5.https://doi.org/10.1002/jor.24752
Source: Revision of a loose cup due to massive circumferential acetabular osteolysis from polyethylene wear, using a custom 3D-printed cup - Complex Hip Surgery - CASE 15
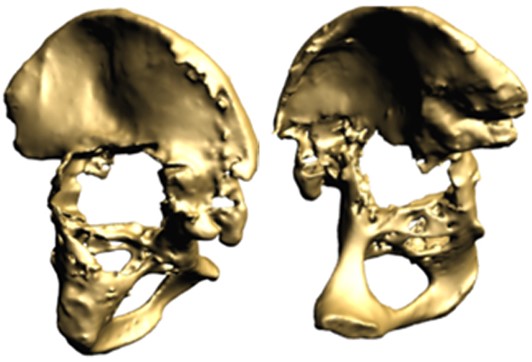
A middle-aged patient came to the clinic with severe pain and limited mobility in his left hip. Previously, he had undergone bilateral hip replacements that included modular necked femoral stems with ceramic-on-ceramic (CoC) bearings. However, the modular design led to corrosion between the titanium femoral stem and the cobalt-chromium neck, causing metal debris and an adverse tissue reaction in his left hip.
The challenge was in addressing the corrosion-related inflammation without exacerbating the damage to the surrounding bone, as the femoral stem was well fixed. Unlike cases with pseudotumors, the patient’s problem originated from metal debris due to the interaction of different alloys in the modular components.
Imaging studies confirmed the presence of metal debris and inflammation around the implant, particularly affecting the left hip. Despite the ceramic-on-ceramic bearing being intact, the corrosion at the modular junction between the neck and the stem was the main culprit. The diagnosis was an adverse reaction to metal debris, secondary to modular neck corrosion.
The surgery was successful, and at his six-week follow-up, the patient reported pain-free mobility and had resumed his daily activities. Imaging showed that the new primary stem had successfully integrated with the bone. At the two-year follow-up, the patient had a well-functioning hip, with no complications and clear evidence of bone growth around the implant, confirming the efficacy of the surgical approach.
This case represents ALTR with CoC. ALTR was characterized by tissue inflammation and extensive fluid accumulation around the ceramic implants. However, ALTR was not caused by the ceramic implant but by corrosion, which occurred between the titanium femoral stem and the cobalt-chromium neck.
Source: Revision of a well-fixed femoral stem with adverse reaction to metal debris from modular neck corrosion, using a non-modular stem — Complex Hip Surgery - CASE 24
References
1. Willert HG, Buchhorn GH, Fayyazi A, et al. Metal-on-metal bearings and hypersensitivity in patients with artificial hip joints. A clinical and histomorphological study. J Bone Joint Surg Am. 2005;87(1):28-36. doi:10.2106/JBJS.A.02039pp.
2. Campbell P, Ebramzadeh E, Nelson S, Takamura K, De SK, Amstutz HC. Histological features of pseudotumor-like tissues from metal-on-metal hips. Clin Orthop Relat Res. 2010;468(9):2321-2327. doi:10.1007/s11999-010-1372-y.
3. Svensson O, Mathiesen EB, Reinholt FP, Blomgren G. Formation of a fulminant soft-tissue pseudotumor after uncemented hip arthroplasty. A case report. J Bone Joint Surg Am. 1988;70(8):1238-1242.
4. Mastel M, Boisvert A, Moore R, Sutherland F, Powell J. Metallosis following hip arthroplasty: two case reports. J Med Case Rep. 2022;16(1):115. doi:10.1186/s13256-022-03336-4.
5. Nabet A, Sax OC, Nace J, Delanois RE, Peroutka RM. Liner dissociation and acetabular erosion treated by implant retention and dual-mobility liner cementation: a case report. JBJS Case Connector. 2022;12(3):e22.00348. doi:10.2106/JBJS.CC.22.00348.
6. Movassaghi K, Patel A, Miller I, Levine BR. An atypical adverse local tissue reaction after ceramic-on-ceramic primary total hip arthroplasty. Arthroplast Today. 2022;14:71-75. doi:10.1016/j.artd.2022.01.025.
7. Diaz Dilernia F, Latorre MR, Comba FM, Zanotti G, Slullitel PAI, Buttaro MA. Adverse local tissue reaction associated with ceramic-on-metal bearing surface in primary total hip arthroplasty: report of two cases. Arthroplast Today. 2022;16:63-67. doi:10.1016/j.artd.2022.04.014.
8. Hall DJ, Pourzal R, Jacobs JJ. What surgeons need to know about ALTR in THA. J Arthroplasty. 2020;35(6S):S55-S59. doi:10.1016/j.arth.2020.01.016.
9. Mistry J, Chughtai M, Elmallah RK, et al. Trunnionosis in total hip arthroplasty: a review. J Orthop Traumatol. 2016;17(1):1-6. doi:10.1007/s10195-016-0391-1.
10. Thapa P, Euasobhon P. Chronic postsurgical pain: current evidence for prevention and management. Korean J Pain. 2018;31(3):155-173. doi:10.3344/kjp.2018.31.3.155.
11. Amstutz HC, Le Duff MJ, Johnson AJ. Socket position determines hip resurfacing 10-year survivorship. Clin Orthop Relat Res. 2012;470(11):3127-3133. doi:10.1007/s11999-012-2347-y.
12. Vendittoli PA, Riviere C, Hirschmann MT, Bini S. Why personalized surgery is the future of hip and knee arthroplasty: a statement from the Personalized Arthroplasty Society. EFORT Open Rev. 2023;8(12):874-882. doi:10.1530/eor-22-0096.
Case Reports